Abstract:
This article introduces the establishment of rheumatoid arthritis (RA) animal models by Jennio. RA is a chronic autoimmune disease with high teratogenic rate and morbidity, characterized by joint synovitis and destructive lesions. To study its etiology and develop effective treatments, reliable animal models are crucial. Common models include Adjuvant Arthritis (AA), Collagen-induced Arthritis (CIA), and Collagen Antibody-Inducible (CAIA), using strains like Lewis, SD, and DBA/1. The article outlines model establishment steps, such as emulsifying type II collagen with adjuvants and immunization methods, noting that while current models are reliable, they still differ from human RA and require further research.
Details:
Establishment of animal models of rheumatoid arthritis
Rheumatoid arthritis (RA) is a chronic, autoimmune disease characterized by joint synovitis and destructive joint lesions, with teratogenic and morbidity rates extremely high. (Recommended reading: Rheumatoid arthritis (RA) model , MH7A rheumatoid arthritis synovial fibroblasts , HFLS-RA human rheumatoid arthritis fibroblast-like synoviocytes )
The clinical symptoms are mainly joint swelling and pain all over the body And movement disorders, etc., the condition is extremely serious and may even lead to disability.
The basic pathological changes are synovitis, synovial swelling, exudation, and neutrophil infiltration in the acute phase; hyperplasia and hypertrophy of the synovial membrane in the chronic phase, forming pannus; the latter is the cause of joint destruction, joint deformity, dysfunction, and disease Enter the pathological basis of the irreversible stage.
Pathogenesis
RA is a complex immune disease, the pathogenesis is not yet fully understood.
At present, it is mostly believed that this disease belongs to an autoimmune disease, and its initiating factor is still unclear. It may be that after infectious agents (such as viruses, mycoplasma or bacteria, etc.) enter the human body, certain components (such as oligosaccharides or Peptide fragments) are taken up by intra-articular synoviocytes and combined into proteoglycans synthesized by synoviocytes to change their structure and become antigenic.
In addition, it is also related to genetic factors, and susceptibility genes for RA have been found.
Objective
To find out the etiology, pathology, immunology and clinical mechanism of rheumatoid arthritis (RA), and find a more effective treatment for RA.
Therefore, it is necessary to find an animal model that is similar to human RA, easy to establish, relatively economical, and can fully reflect the characteristics of RA.
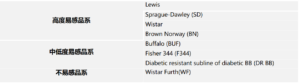
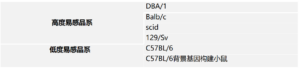
(1) Adjuvant Arthritis (Adjuvant Arthritis, AA) (recommended reading: Adjuvant Induced Arthritis (AIA) rodent model )
AA was first created by bacteriologist Freund in the 1950s, also known as Freund’s Adjuvant agent arthritis. Usually complete Freund’s adjuvant (CFA) is used as mediating solvent.
The mechanism is that the arthritis antigen caused by Mycobacterium tuberculosis is 65 kD heat shock protein (HSP), and the cartilage of RA patients has proteoglycan bridging protein antigen components similar to 65 kD HSP. CFA injection activates T cells, and activated T cells participate in the pathogenesis of RA .
(2) Collagen-induced arthritis (CIA) (recommended reading: Collagen-induced arthritis (CIA) rodent model )
The CIA model is an experimental arthritis animal model first established by Trentham et al. in 1977.
Type II collagen was mixed with complete Freund’s adjuvant (CFA) until completely emulsified to prepare type II collagen emulsion for immunization of animals.
The modeling mechanism is that 50% of RA patients have autoantibodies against CⅡ in serum, indicating that CⅡ can induce an autoimmune response of arthritic nature in vivo.
(3) Collagen antibody-inducible (CAIA)
anti-type Ⅱ collagen monoclonal antibodies were derived from 8-week-old male DBA/1J mouse CIA models, and these antibody mixtures could directly act on type Ⅱ after injection into the joint cavity of the model mice. Collagen or other self-antigens that are highly expressed in the body play an immune-mediated role.
The clinical symptoms of this model are very similar to those of CIA and RA, and the outstanding features are rapid onset within a few days and infiltration of macrophages and multinucleated leukocytes in joint tissues. This model well reflects the severe joint damage induced by exogenous antigen-antibody stimulators.
Preparation of Type II Collagen Emulsion
Using a high-speed homogenizer to stir the adjuvant and collagen solution (1:1), the order of addition is to add the aqueous solution to the oil solution, and add drop by drop during stirring.
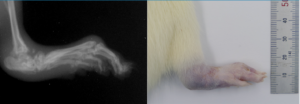
Successful demonstration of model construction
Summary
To reduce collagen denaturation caused by heat during shaking, another tube containing ice-water mixture can be placed outside the tube. Stirring time is about 2min.
After the collagen adjuvant is made into an emulsion, the quality of the emulsion must be checked. Immunization can only be carried out if the emulsified collagen is dripped into water and does not diffuse. The emulsion is prepared and used immediately, and the storage time of the emulsion should not exceed 1 hour.
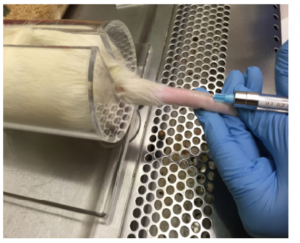
Footpad immunization
The needle should be inserted under the skin of the footpad pointing towards the ankle: this ensures drainage of the adjuvant to the lymph nodes. A severe acute inflammatory reaction will be seen within 30 minutes, the peak period is 3-4 days, and usually lasts for 20-25 days.
The immunized hindpaw was not used as a scoring criterion because the immunized hindpaw was swollen even though none of the extremities were swollen.
Swelling occurred in the uninjected paw 12-14 days after immunization, peaked at 2-3 days, and arthritis lasted 20-25 days. However, some rats will develop chronic bony hypertrophy caused by periosteal reaction.
The base of the tail was immunized with
2mg/ml chicken type II collagen and 1:1 emulsified with complete Freund’s adjuvant containing 5mg/ml inactivated Mycobacterium tuberculosis, and 200ul intradermally injected at the base of the tail, and 21 days later, 2mg/ml chicken type II collagen was used After emulsifying with incomplete Freund’s adjuvant 1:1, intradermal injection of 100ul for the second time at the base of the tail
In order to further study rheumatoid arthritis, establishing a reliable model is the key to research. The current RA model
cannot fully reflect the clinical symptoms of human beings, and there are certain differences. Among the existing models, the collagen-
induced model and the adjuvant model are relatively It is more reliable and needs to be further explored.