Abstract:
This article states that the World Health Organization shows about 240 million people worldwide are infected with HBV. A study in *Nature-Communications* finds HBV integrates its DNA into liver cells early in tumor development, causing abnormal cell proliferation. It randomly integrates into chromosomes, most frequently into the TERT gene on 5p, and can lead to large – fragment gene loss, like telomere deletion, damaging tumor suppressor genes such as TP53. This integration occurs years before HCC diagnosis, even 21 years earlier, increasing cancer risk.
Details:
According to the World Health Organization, approximately 240 million people worldwide are infected with the hepatitis B virus ( HBV ). The virus not only affects the chromosomes of liver cells, but may even lead to hepatocellular carcinoma.
Recently, a study in “Nature-Communications” found that HBV quietly promotes the growth and survival of cancer cells. These viruses will integrate their own DNA into liver cells in the early stage of tumor development, resulting in abnormal proliferation of liver cells. This damage to the DNA of normal cells can occur as early as 21 years before the cancer is diagnosed.
The researchers obtained data from 296 HCC samples from the sample bank of the Genome-wide Pan-Cancer Analysis Project. By comparing with normal blood samples, they found that 51 tumor samples showed HBV DNA, and all viral integration events occurred 148 times.
The analysis revealed that the integration of the viral DNA was random and could occur on either chromosome. Among all the integration events, the TERT gene on chromosome 5p had the highest occurrence frequency, 11 occurred directly on the TERT gene, and 9 occurred upstream of the gene.
▲The gene of HBV may be integrated into any position (Source: Reference [2])
Many previous studies have found that mutations in the TERT gene are associated with an increased risk of various cancers, and abnormalities in this gene can damage the maintenance end of cells normal functioning of the granules, eventually causing DNA damage. The new study once again confirmed that the TERT gene is also the most important integration target of HBV.
Other oncogenes (gene coding region and nearby) modified by HBV integration include KMT2B and CCNE1, which are located on chromosome 19q.
In addition to directly inserting genes, HBV may also cause more serious loss of large fragments of genes, which occurred in 23 tumor genes. The study speculates that this large area of gene loss is also an important reason for the development of cancer.
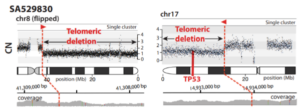
Further analysis found that this virus integration event basically appeared in the early stage of tumor development, and could even be traced back to many years before the patient was diagnosed with hepatocellular carcinoma. One of the samples was even more surprising. 21 years before the patient was diagnosed with cancer, HBV recombination occurred on chromosome 10 of the sample, accompanied by the loss of the telomere region.
This phenomenon of telomere deletion often occurs in the process of HBV recombination. Studies have pointed out that this will lead to impairment of the function of some tumor suppressor genes. For example, the key tumor suppressor gene TP53 may lose one copy, while the other copy may also be mutated . In this way, without the protection of tumor suppressor genes, the risk of cell canceration will be significantly increased.
▲Tumor suppressor genes may be damaged (picture source: Reference [2])
Overall, in the 23 hepatocellular carcinoma samples with telomere deletion alone, there are about 244 genes listed as tumor suppressor-related genes have been deleted, or become loss-of-function genes. According to the CancerGene Census database, 37% of these genes have been found to be associated with HCC.
HBV, as one of the few viruses that can be associated with cancer, has been identified as capable of causing large fragments of damage in the genome. Next, research will focus on the long-term effects of the virus on non-cancerous tissue.
Note: The original text has been deleted.
References:
[1] Hepatitis B virus can trigger genetic changes in liver cells years before cancer diagnosis. Retrieved Nov 29th, 2021 from https://medicalxpress.com/news/2021-11-hepatitis-virus- trigger-genetic-liver.html
[2] Eva G. ?lvarez et al, Aberrantintegration of Hepatitis B virus DNA promotes major restructuring of human hepatocellular carcinoma genome architecture, Nature Communications (2021).DOI: 10.1038/s41467- 021-26805-8